CLIFT NOTES all rights reserved
The "F*#%" Word Series Part 3
PHYSICAL THERAPY FRAUD, ABUSE and WASTE
“We must understand that the problem begins at home and that we must collectively prove our value to society. We must produce better outcomes than the pretenders do.”
This quotation was embedded in an article that cited real life examples of physical therapy fraud, abuse and waste as it occurred in outpatient settings. Here is a sampling:
59 consecutive ultrasound applications to the cervical spine of a 3 yr-old for ‘migraine headaches’
560 “work hardening” sessions, 14 separate CPT codes daily, $500.00-$600.00 per session. Discharge goal: for 71 yr. old patient was to military press/overhead 150# painfree.
Dx: grade 1 rotator cuff strain, job-letter courier, Total billed: &160,000 dollars.
10 yrs of daily PT for lumbar strain/sprain, Texas workers compensation case
292 consecutive cold laser applications (an FDA experimental device)without informed consent
Land-based therapy and aquatic therapy in same session in a group setting but billed as individualized programs
Fortunately, these examples are outliers however they may be the first impressions that others have of this profession. First impressions can become permanent ones and, we only get one. Because of the relative youth and obscurity of the PT profession, the impact of unscrupulous providers is potentially greater.
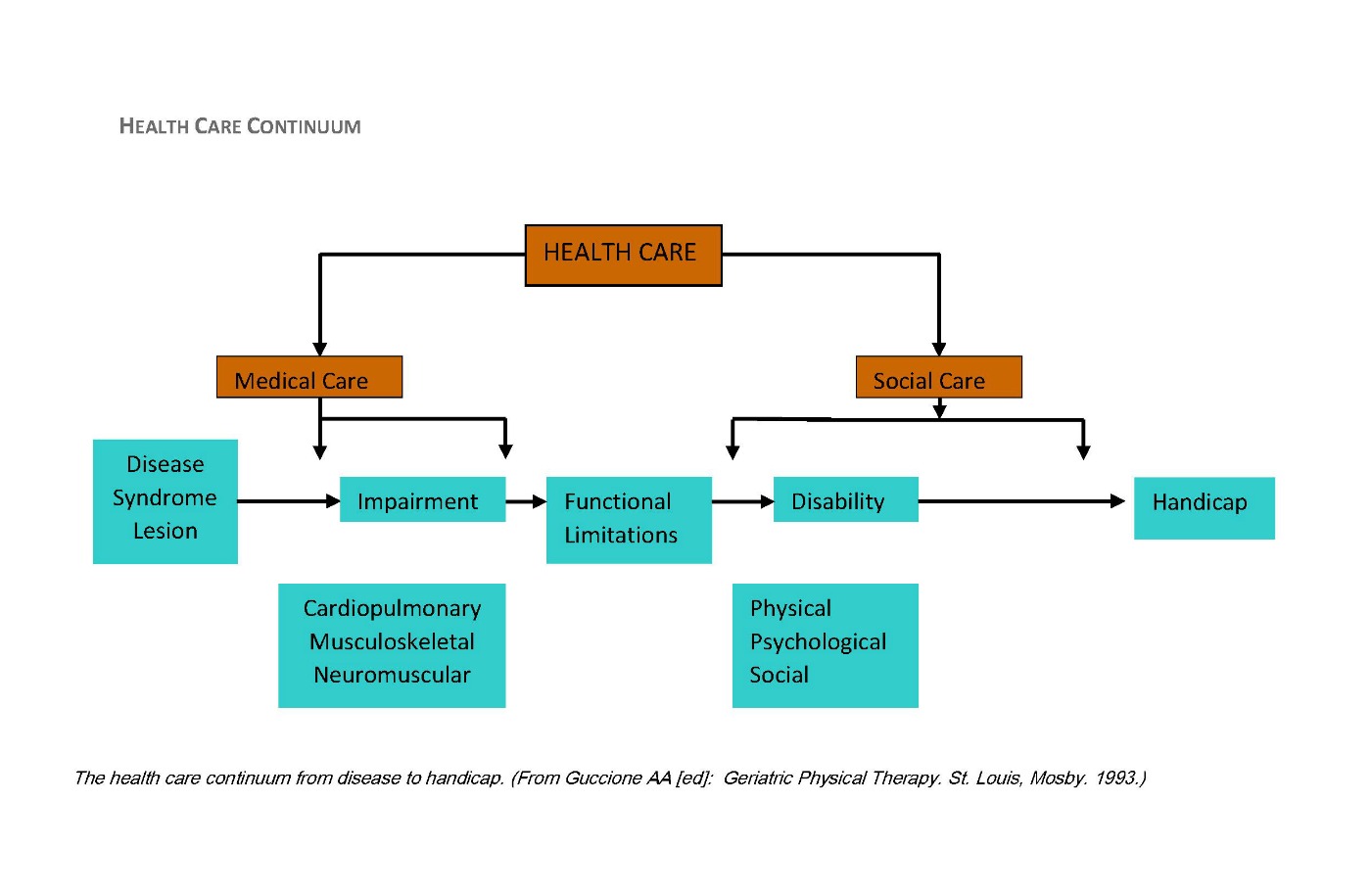
Physical therapy through much of the twentieth century was an unknown or poorly understood profession particularly, among payers. Physical therapy for the most part has been viewed as a discretionary or elective service. Although the growth in primary care physicians as “gatekeepers” continued to grow and the desire of managed care to restrain costs deepened; physical therapy remained in the shadows despite, the value proposition it offers especially, when compared to the costs of hospitalization, surgery and pharmaceuticals. Physical therapists are THE functional therapists (along with our occupational therapy or OT colleagues).
Physical therapy essentially practiced in the shadows of mainstream medicine but by the mid-1980s physical therapy had finally made it onto the radar screens of other healthcare stakeholders. Regrettably, it was often for the wrong reasons. Abusive examples of physical therapy were routinely seen by claims adjusters, case managers, utilization reviewers and employer because PT was viewed as a “cash cow”. The 1980s was defined by a “gold rush” of publicly-traded corporations competing for profits. This was also a time when “pretenders” or many non-physical therapists profusely billed for so-called “PT”.
A Pretender or a PT?
Yes, physical therapy was finally on the radar screen, but for some it looked like an enemy bomber not, the relief ship we know it to be. For skeptics who may believe that “these kinds of cases {examples above don’t exist anymore”, they may be right; in many instances it has gotten worse! It is now common to see millions of dollars of fraud from single clinics or providers (see Part 1 of the Fraud series, May 23, 2016).
This is an ultimate tragedy for the involved patients/clients many of whom have lost control of their medical and legal destinies because they have trusted unscrupulous providers. The late great Jules Rothstein, a physical therapist change agent and former editor of the APTA journal opined that the physical therapy profession would be judged by others through encounters with “average” not, exceptional therapists. In reality, the profession may be judged by our worst therapists and the non-therapist pretenders who masquerade as “physical therapists”. This is a tragedy unfolding at the worst possible time as the physical therapy profession strives to produce only Doctors of Physical Therapy/DPTs by 2020 (APTA Vision Statement 2020).
A vast majority of physical therapists are compassionate, ethical, conscientious, and law abiding healers trying to make a difference in patients’ pain and disability status. The best of physical therapy is on the horizon with the nexus of the millennial generation, evidence-based practice and advances in technology. In the meantime, all health care stakeholders have an ongoing role of eliminating fraud, abuse and waste, which is a cancer of the American healthcare system especially, government-funded programs.
The first and foremost responsibility for combating fraud and abuse resides with physical therapists. Here are some recommended actions that will ultimately serve the needs of our patients while doing no harm.
Identify and report fraud, abuse and waste when you see it.
Appeal only legitimate cases when you are denied reimbursement that is supported by evidence and sound outcomes documentation.
Embrace don’t resist pre-authorization of services, its good risk management.
Educate payers through your clinical documentation, websites, blogs, presentations and other media.
Distinguish physical therapist from the generic label “physical therapy”.
Share studies that support your treatment interventions especially, randomized control trials, meta-analysis and patient/client testimonials.
Perform peer review both internally and for payers.
Contact licensure boards to report aberrant behaviors and unscrupulous providers.
Use the correct codes (Medicare’s Correct Code Initiative)
Provide documentation that explains how extenders of care are supervised and task delegated to them.
Liberally distribute APTA educational materials (e.g. Core documents, Code of Ethics) and bring special circumstances to the attention of APTA practice, reimbursement and legal staff.
Educate your referral sources that Physical Therapists are autonomous practitioners who perform independent evaluations/re-evaluations, formulate “physical therapy” diagnoses, develop plan of care with treatment goals, and ultimately determine when and why to discharge a patient from PT. In 36 years of peer review experience the number one excuse/alibi that treating therapists when questioned about overutilization express is; “the doctor keeps referring the patient to me” or “the doctor wants PT to continue”. A therapist cannot have it both ways meaning out of one side of their mouth they assert that they are autonomous practitioners then use the referrer as the scapegoat when over-utilization of services occurs or bills are questioned.
Know when ‘restorative care” becomes ‘maintenance care’ or when the patient has reached a functional plateau. If a ‘maintenance program’ is medical necessary, provide the evidence to support it. Hint, read the health plan exclusions and limitations sections.
Clearly documented what constitutes ‘group vs individual’ treatment, ‘work conditioning vs work hardening’, clinically required therapeutic exercises and home exercise plans/HEPs, clinic-based thermal agents vs home heat/ice.
Provide an educated, evidence-based estimate of total treatment duration and costs. Be prepared to explain outlier or complex cases. Justify the use of the “55” modifier code.
Become an exceptional master clinician and employ only the best so that physical therapists are no longer judged from the standard of “average” therapists.
In the mid-1990s I was invited by the American Physical Therapy Association to author an ongoing column entitled “Utilization Review” in PTMagazine. I had been involved in physical therapy peer review since 1982, when I founded Physical Therapy Review Services or PTRS, to provide “true” peer to peer review, long before it was required by statute.
There were two primary motives that spurred me to explore beyond the clinical box and venture into the unknown waters of PT review. One, relatively few people truly understood what physical therapists were trained and educated to do. The 1965 federal Department of Labor in its Dictionary Occupational Titles essentially described physical therapy as a local modality-laden profession, which some inaccurately describe to this day, as “passive modalities”. Clearly, the definition was grossly outdated and in need of reform to reflect the vital role PT served in human movement and function via therapeutic exercises. The fourth edition of DOT arrived in 1995. Secondly, physical therapy cost containment was being performed by claims adjusters, nurses, physicians and even laypersons; as was the case with a Florida-based UR company that enrolled high school graduates in a 6-week “PT UR University”. These so-called reviewers produced one page boiler plate “denials” (rarely if ever did they identify under-utilization), which resulted in a printing press for $150.00 bills for services rendered. Physical therapists with relatively few exceptions (The FOTO Group, under Mary Foto, OT, AOTA past president had performed Medicare OT/PT reviews) were not involved with PT peer to peer review especially in the outpatient arena where the profession and costs were exploding. The Workers’ Compensation Research Institute/WCRI in 1994 had identified chiropractic and physical therapy costs as the two greatest cost drivers of the medical component. A year later the General Accounting Office/GAO published, “Tighter Rules Needed to Curtail Overcharges for Therapy in Nursing Homes”. HHS Secretary Donna Shalala reported $10 dollars in recoveries for every $1 dollar spent on the joint federal-state government collaboration known as “Operation Restore Trust”, directed at Medicare & Medicaid fraud, abuse and waste in nursing homes. This was the impetus for statistical methods to target providers for investigations and audits, which continues today with greater intensity.
Two articles were penned with the expressed goal of challenging physical therapists to do some house cleaning and differentiate physical therapist delivered care from physical therapy, which was quickly becoming a generic term (“PT on the Radar Screen” and “Tolerated Treatment Well May No Longer Be Tolerated”, D.W. Clifton, PT). It was apparent that PT’s heightened visibility particularly on payer radar screens would not be without its costs.
In conclusion, providers and payers are highly dependent on one another and mutual survival or destruction may be assured by whether they view one another as adversaries or partners in health. Both sectors engage in contracts with patients/beneficiaries to whom they owe certain duties (business and/or clinical). Payers need providers to serve in a risk management capacity while providers require payers for fiscal survival as private pay is not an option for the vast majority of patients. Partnerships must be forged between all stakeholders to combat fraud, abuse and waste, which all of us pay for but relatively few engage in.
Stayed tuned for Part 4 of the “F” word/Fraud series; “PT-PreTenders”.